A trace element that 's the real deal. That is how iron could be described. From oxygen supply to energy production, it is involved in numerous vital processes in your body. However, not everyone has enough of it available – iron deficiency is one of the most common deficiency symptoms.
The symptoms that can accompany it are varied. At the same time, however, there are several ways to remedy such iron deficiency. We have therefore summarised everything you need to know about this topic and will work with you to get to the bottom of the pressing question: Iron deficiency – what should you do now?
Definition: What is iron deficiency?
Let's start with the definition: what exactly is iron deficiency? Well, this deficiency occurs when there is too little iron in the blood, which affects your body in various ways.
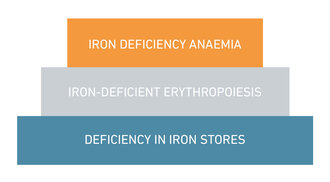
If you find yourself in this situation, your body can initially draw on its internal iron stores. However, once these reserves are depleted, it becomes dangerous because anaemia sets in. This means that not enough haemoglobin and ultimately not enough red blood cells can be produced. Not only does blood formation falter, but several other iron-dependent bodily functions are also disrupted.
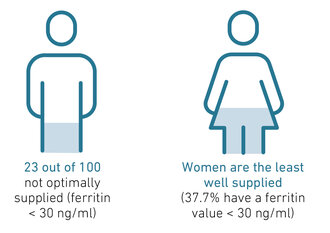
Approximately one third of the world's population is affected by iron deficiency, and it has also been found that iron deficiency without anaemia is more common in Western countries than iron deficiency with anaemia (iron deficiency anaemia) – this form affects up to 20% of the population.
What causes iron deficiency?
Iron deficiency occurs when you consume more iron than your body has available. This can have several causes: many people develop iron deficiency because they consume too little of this trace element in their diet, while others develop this disorder due to reduced iron absorption in the small intestine. An increased iron requirement (e.g. pregnancy, sport) or increased iron loss through bleeding (e.g. severe menstrual bleeding, stomach ulcers) can also trigger iron deficiency. As a rule of thumb, you lose approximately 0.5 mg of iron per 1 ml of blood.
Iron is often a “woman's issue”
This brings us to another important topic: iron is considered THE trace element for women. This is not surprising, as women need more iron than men for about half their lives – from puberty to menopause – due to menstruation. But the fact is that not every woman manages to get the necessary amount. This is shown by the BIOGENA Good Health Study*: 37.7% of the women who took part suffered from iron deficiency (ferritin 30 ng/ml). In comparison, only 5.8% of men had such a deficiency.

Iron deficiency during pregnancy and breastfeeding
Pregnancy and breastfeeding are particularly demanding phases for women. They are also considered high-risk periods for developing iron deficiency. The reason: not only the expectant mother, but also the growing child needs a lot of this trace element during this time. In addition, the enlarged uterus and placenta must be supplied with iron. And afterwards? Even during breastfeeding, women need more iron than usual. On the one hand, the losses from pregnancy and childbirth must be compensated for, and on the other hand, the child is also supplied with iron via breast milk.
Iron deficiency & menopause
Women who are approaching menopause should also keep an eye on their iron levels. This is because hormonal changes can lead to heavy menstrual or intermenstrual bleeding, which depletes iron stores. Once menstruation finally stops (menopause), the situation for affected women usually improves and their iron requirements become similar to those of men (10 mg of iron per day).
Iron deficiency in children
Iron deficiency does not spare even the youngest children. During periods of rapid growth, this trace element is needed to maintain normal bodily functions and increase blood volume. In adolescents, an unbalanced diet low in iron, combined with food intolerances or an iron absorption disorder, often leads to such a deficiency later in life. Parents who suspect their child has an iron deficiency should therefore act quickly and seek professional help.
Iron deficiency & sport
Iron deficiency and sport – this combination is also not uncommon. The reason: physical exertion and increased sweating mean that your body needs more iron. And the more strenuous the sport, the greater the loss, because your body loses around 0.5 milligrams of iron with every litre of sweat. In addition, high levels of physical activity lead to increased production of the iron-containing red blood pigment haemoglobin, which is needed for the formation of red blood cells (erythrocytes) and the muscle protein myoglobin.
How does this affect you? Especially if you do endurance or competitive sports, you may find that you are not achieving the desired training results. You should therefore have your iron levels checked regularly.
Iron deficiency & nutrition
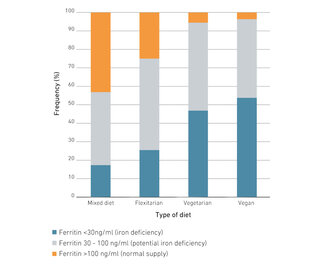
Want to have sufficient iron and energy? This is fundamentally possible even without meat. Nevertheless, people who rely on a plant-based diet often find it more difficult to get enough iron. This is also confirmed by our BIOGENA Good Health Study*. While 43.6% of mixed-diet eaters and 25.6% of flexitarians had an optimal iron supply, only 5.6% of vegetarians and 3.8% of vegans were in the optimal range. In addition, more than half of vegans (53.8%) and almost half of vegetarians (47.2%) had a clear iron deficiency (ferritin 30 ng/ml).

Iron deficiency symptoms, signs & consequences
Energy levels close to zero? Pale Snow White complexion? Ice-cold hands? No doubt about it – these are typical symptoms that can indicate iron deficiency. But that's not all! Because iron deficiency has many faces.
Even in the early stages, you may feel particularly tired, your performance may decline and you may suffer from hair loss. If the iron deficiency progresses (stage 2), other symptoms will appear. These include dry skin, skin blemishes, cracks in the corners of the mouth, susceptibility to infections, sensitivity to cold or concentration problems.
In stage 3, your iron stores are so depleted that it leads to serious disturbances in blood formation. Not only does the number of red blood cells (= erythrocytes) decrease, but their haemoglobin content also decreases. Other symptoms of this advanced stage include pale skin, headaches, dizziness and physical and mental decline.

Symptoms at a glance:
| Neurological symptoms: • Tiredness and fatigue • Headaches • Declining capacity for thought • Forgetfulness • Concentration disorders • Sleep problems |
Skin, hair & nails: • Brittle nails • Hair loss • Dry skin • Cracks at the side of the mouth • Cracked lips • Pale skin and mucous membranes |
| Mental factors: • Depressed mood • Restlessness • Tension • Attention deficit disorders |
Musculoskeletal system: • Muscle weakness • Rapid fatigue • Reduced performance • Restless legs syndrome |
| Nutrition: • Loss of appetite |
Cardiovascular system and lungs: • Anaemia (iron deficiency anaemia) • Palpitations • Dizziness • Shortness of breath • Feeling of cold • Exhaustion |
| Immune defence: • Increased susceptibility to infection |
Detecting iron deficiency
Do you suspect that you may be suffering from iron deficiency? If so, have a laboratory blood test carried out – this will provide clarity. But what do you need to bear in mind here?
Iron levels: When can we say that there is an iron deficiency?
When iron deficiency is suspected, the haemoglobin level is often measured first. This provides information about how much iron is contained in the blood. The catch: it does not reveal the overall state of your body's iron stores. For an accurate determination of iron status, ferritin levels, transferrin levels and transferrin saturation should also be checked. All these values must be within the normal range.
Normal values and deviations
| Deficiency | Normal values | Excess | |
| Ferritin (in ng/ml) | < 30 | 30-300 | > 1000 |
| Transferrin (mg/dl) | > 400 | 200 – 400 | < 200 |
| Transferrin saturation (%) | < 16 | 16-45 | > 45 |
Vitamin B12 and/or iron deficiency?
What many people don't know: A simultaneous iron and vitamin B12 deficiency can cause problems with diagnosis. This is because iron deficiency in the blood count can sometimes mask a B12 deficiency – and vice versa. The reason: iron and vitamin B12 are both important for blood formation, which is why the symptoms of a deficiency are similar. If a combined deficiency is suspected, more detailed laboratory tests should therefore be carried out.
Fixing iron deficiency: What you can do now
Are you suffering from iron deficiency and wondering what to do now? Then it's best to consult a health expert to find out the cause. Whether it's malnutrition, heavy periods or impaired iron absorption – if you know the reason, you can take better countermeasures.
In this case, you should primarily focus on an iron-rich diet. You can also take high-quality iron supplements to replenish your stores and remedy your iron deficiency.
How long does it take to remedy iron deficiency?
For the treatment of iron deficiency or even iron deficiency anaemia, you should expect it to take several weeks to months. If you are taking iron supplements over a longer period of time, regular laboratory diagnostic analysis is also recommended to ensure the correct dosage.
How much iron per day for iron deficiency?
The amount of iron per day that is appropriate for iron deficiency varies from person to person. Consult a healthcare professional – they can assess your current status and advise you on the appropriate dosage. Current guidelines recommend high doses of bivalent iron salts (50 to 100 mg per day). However, if you have problems with high-dose iron salt supplements, you should take a closer look at low-dose, special herbal extracts (such as those found in MoFerrin® 21). Studies confirm that these can also be effective and represent an effective and well-tolerated alternative to the usual high-dose iron salts.
Supplements for iron deficiency: tablets, capsules, liquid iron, etc.
To remedy iron deficiency, you can choose from a variety of iron supplements, ranging from tablets and granules to liquid products. The choice depends primarily on your individual preferences. While some people prefer a tasty iron juice, others prefer tasteless, convenient capsules. Whatever you choose, make sure that the supplements do not contain any unnecessary additives.
Conclusion: Widely used, but often misunderstood
Iron deficiency is widespread worldwide – and yet often goes unrecognised. If you struggle to get out of bed in the morning and feel like you can't perform at your best physically or mentally, you should have your iron levels checked and, if necessary, give your body a boost with more iron. This is a quick way to remedy or prevent iron deficiency. More iron means more vitality!
* About the BIOGENA Good Health Study
With 1,377 participants, the BIOGENA Good Health Study is Europe's most comprehensive study on micronutrients, health and well-being. The aim of this large-scale study was to provide an up-to-date picture of the health and nutritional status of the Austrian population and to demonstrate that a better micronutrient supply is rewarded with increased physical and mental well-being.
Frequently asked questions about iron
Iron deficiency is generally easily treatable. In addition to an iron-rich diet, iron preparations can replenish your iron stores.
Iron deficiency impairs the iron-dependent functions of the body. While blood formation is not impaired at the beginning, advanced "manifest" iron deficiency also causes serious disorders with blood formation.
Typical symptoms of iron deficiency anaemia are fatigue, paleness, dizziness and a deterioration in physical and mental performance. Non-anaemic symptoms occur more frequently and earlier than symptoms of iron deficiency anaemia, such as skin and nail changes, hair loss, burning mouth syndrome or susceptibility to infection.
Symptoms that indicate iron deficiency (e.g. fatigue, concentration problems, loss of performance) may also occur in the course of other nutrient deficiencies or diseases. A laboratory diagnostic analysis is therefore indispensable to detect iron deficiency.
The combination of iron-rich foods – so-called “iron boosters” – can improve iron absorption into the body. Iron boosters are foods that contain vitamin C, vitamin A, fruit acids, lactic acids or sulphur-containing amino acids.
Sources:
Fachgesellschaft für Ernährungstherapie und Prävention e.V. 2023. Eisen – Ernährungstherapeutische Aspekte. Stand Juni 2023. https://fet-ev.eu/eisen/ , zugegriffen 28.8.2023
Nielsen P. 2016. Diagnostik und Therapie von Eisenmangel mit und ohne Anämie. 2. Auflage. Bremen: UNI-MED Verlag AG; 2016.
Bergmann K. 2018. Anämie und Eisenmangel: Neue Norm- und Grenzwerte für Kinder und Jugendliche. Zeitschrift Pädiatrie. 2018; 5:25-32.
Brunner-Agten S, Meyer MK, Huber, AR. 2012. Eisenmangel, Gehirnentwicklung und kognitive Leistungsfähigkeit. Schweitzer Zeitschrift für Ernährungsmedizin. 2012; 3:28-35.
Hahn A, Ströhle A, Wolters M. Ernährung: Physiologische Grundlagen, Prävention, Therapie. 3. Auflage. Stuttgart: Wissenschaftliche Verlagsgesellschaft; 2016.
Biesalski, 2017. Taschenatlas der Ernährung. Georg Thieme Verlag KG.
Deutsche Gesellschaft für Ernährung e.V. (DGE). 2023. Referenzwerte: Eisen. https://www.dge.de/wissenschaft/referenzwerte/eisen/?L=0, zuletzt aufgerufen in
Hastka J et al. 2022. Eisenmangel und Eisenmangelanämie. Onkopedia Leitlinien. Stand: Juli 2022. https://www.onkopedia.com/de/onkopedia/guidelines/eisenmangel-und-eisenmangelanaemie/@@guideline/html/index.html, zugegriffen 29.8.2023
Yiannikourides A, Latunde-Dada G.O. 2019. A Short Review of Iron Metabolism and Pathophysiology of Iron Disorders. Medicines 2019, 6(3), 85.
Wallace D.F. 2016. The Regulation of Iron Absorption and Homeostasis. Clin Biochem Rev. 2016 May; 37(2): 51-62.
Lal A. 2019. Iron in Health and Disease: An Update. Indian J Pediatr. 2019 Sep 13.
Weiss G. 2016. Eisentherapie. Österreichische Ärztezeitung 13/14. 15. Juli 2016.
Lee E.C., Fragala M.S. et al. 2017. Biomarkers in Sports and Exercise: Tracking Health, Performance, and Recovery in Athletes. J Strength Cond Res. 2017 Oct; 31(10): 2920–2937.
Milman N et al. 2017. Iron status in pregnant women and women of reproductive age in Europe. Am J Clin Nutr. 2017 Dec;106(Suppl 6):1655S-1662S.
Breymann C., Auerbach M. 2017. Iron deficiency in gynecology and obstetrics: clinical implications and management. Hematology Am Soc Hematol Educ Program. 2017 Dec 8; 2017(1): 152–159.
Fernández-Gaxiola AC, De-Regil LM. 2019. Intermittent iron supplementation for reducing anaemia and its associated impairments in adolescent and adult menstruating women. Cochrane Database Syst Rev. 2019 Jan 31;1:CD009218.
Shoemaker ME,et al. 2019. High Prevalence of Poor Iron Status Among 8- to 16-Year-Old Youth Athletes: Interactions Among Biomarkers of Iron, Dietary Intakes, and Biological Maturity. Am Coll Nutr. 2019 Jul 24:1-8.
Low M.S. et al. 2016. Daily iron supplementation for improving anaemia, iron status and health in menstruating women. Cochrane Database Syst Rev. 2016 Apr 18;4:CD009747.
Merwe L.F., Eussen S.R. 2017. Iron status of young children in Europe. Am J Clin Nutr. 2017 Dec; 106(Suppl 6): 1663S–1671S.
Parisi F et al. 2017. Effects of different regimens of iron prophylaxis on maternal iron status and pregnancy outcome: a randomized control trial. J Matern Fetal Neonatal Med. 2017 Aug;30(15):1787-92.
Aporta RR, et al. 2016. Retrospective case reports of anemic pregnant women receiving intravenous ferric carboxymaltose: Experience from a tertiary hospital in Spain. Obstet Gynecol Int. 2016 Aug;5060252:1-5.
Joo EY et al. 2016. Iron deficiency anemia in infants and toddlers. Blood Res. 2016 Dec;51(4):268-73.
Wei S et al. 2019. Increased hepcidin expression in adipose tissue as a primary cause of obesity-related inhibition of iron absorption. J Biol Regul Homeost Agents. 2019 Jul-Aug;33(4):1135-1141.
Lam LF, Lawlis TR. 2017. Feeding the brain - The effects of micronutrient interventions on cognitive performance among school-aged children: A systematic review of randomized controlled trials. Clin Nutr. 2017 Aug;36(4):1007-1014.
Milman N, et al. 2014. Ferrous bisglycinate 25 mg iron is as effective as ferrous sulfate 50 mg iron in the prophylaxis of iron deficiency and anemia during pregnancy in a randomized trial. J Perinat Med. 2014 Mar;42(2):197-206. doi: 10.1515/jpm-2013-0153.
Bagna R et al. 2018. Efficacy of Supplementation with Iron Sulfate Compared to Iron Bisglycinate Chelate in Preterm Infants. Curr Pediatr Rev. 2018;14(2):123-129.
Fäth-Neubauer B., Viebahn I. 2012. Biogena Eisen-Interventionsstudie: Pflanzliches Eisen füllt Eisenspeicher. Biogena Naturprodukte GmbH.
Fäth-Neubauer B., Viebahn I. 2017. Pflanzliches Eisen ist in physiologischen Dosierungen effektiv. Biogena Naturprodukte GmbH.
Martin, M. 2009. Pflanzenbasiertes Eisen (MoFerrin®) im Vergleich zu einem herkömmlichen Eisenpräparat (Eisen-II-Gluconat mit Ascorbinsäure). GanzImmun Diagnostics AG.
Lönnerdal, B. 2009. Soybean ferritin: implications for iron status of vegetarians. Am J Clin Nutr. 89(5):1680S-1685S.
Theil, E.C. et al. 2012. Absorption of Iron from Ferritin is Independent of Heme Iron and Ferrous Salts in Women and Rat Intestinal Segments. Journal of Nutrition.
Kumar A, Sharma E, Marley A, Samaan MA, Brookes MJ. Iron deficiency anaemia: pathophysiology, assessment, practical management. BMJ Open Gastroenterol. 2022 Jan;9(1):e000759. doi: 10.1136/bmjgast-2021-000759. PMID: 34996762; PMCID: PMC8744124. https://pubmed.ncbi.nlm.nih.gov/34996762/
Pasricha SR, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet. 2021 Jan 16;397(10270):233-248. doi: 10.1016/S0140-6736(20)32594-0. Epub 2020 Dec 4. PMID: 33285139. https://pubmed.ncbi.nlm.nih.gov/33285139/
Cappellini MD, Santini V, Braxs C, Shander A. Iron metabolism and iron deficiency anemia in women. Fertil Steril. 2022 Oct;118(4):607-614. doi: 10.1016/j.fertnstert.2022.08.014. Epub 2022 Sep 6. PMID: 36075747. https://pubmed.ncbi.nlm.nih.gov/36075747/
Petraglia F, Dolmans MM. Iron deficiency anemia: Impact on women's reproductive health. Fertil Steril. 2022 Oct;118(4):605-606. doi: 10.1016/j.fertnstert.2022.08.850. PMID: 36182259. https://pubmed.ncbi.nlm.nih.gov/36182259/
Gattermann N, Muckenthaler MU, Kulozik AE, Metzgeroth G, Hastka J. The Evaluation of Iron Deficiency and Iron Overload. Dtsch Arztebl Int. 2021 Dec 10;118(49):847-856. doi: 10.3238/arztebl.m2021.0290. PMID: 34755596; PMCID: PMC8941656. https://pubmed.ncbi.nlm.nih.gov/34755596/
Kumar SB, Arnipalli SR, Mehta P, Carrau S, Ziouzenkova O. Iron Deficiency Anemia: Efficacy and Limitations of Nutritional and Comprehensive Mitigation Strategies. Nutrients. 2022 Jul 20;14(14):2976. doi: 10.3390/nu14142976. PMID: 35889932; PMCID: PMC9315959. https://pubmed.ncbi.nlm.nih.gov/35889932/
Auerbach M, DeLoughery TG, Tirnauer JS. Iron Deficiency in Adults: A Review. JAMA. 2025 May 27;333(20):1813-1823. doi: 10.1001/jama.2025.0452. PMID: 40159291. https://pubmed.ncbi.nlm.nih.gov/40159291/
Kuwabara AM, Tenforde AS, Finnoff JT, Fredericson M. Iron deficiency in athletes: A narrative review. PM R. 2022 May;14(5):620-642. doi: 10.1002/pmrj.12779. Epub 2022 Mar 17. PMID: 35100494. https://pubmed.ncbi.nlm.nih.gov/35100494/
Percy L, Mansour D, Fraser I. Iron deficiency and iron deficiency anaemia in women. Best Pract Res Clin Obstet Gynaecol. 2017 Apr;40:55-67. doi: 10.1016/j.bpobgyn.2016.09.007. Epub 2016 Oct 1. PMID: 28029503. https://pubmed.ncbi.nlm.nih.gov/28029503/